Coastal Research Institute was founded by physicians with a focus on patient outcomes and community relationships. We offer multi-disciplinary services for clinical research including experimental design, study execution, data analysis, publication and podium.
UPCOMING EDUCATIONAL EVENT
EMPOWER YOU: The Patient Centric Conference
Presented by Coastal Research Institute
August 26, 2023
Town & Country, San Diego, CA
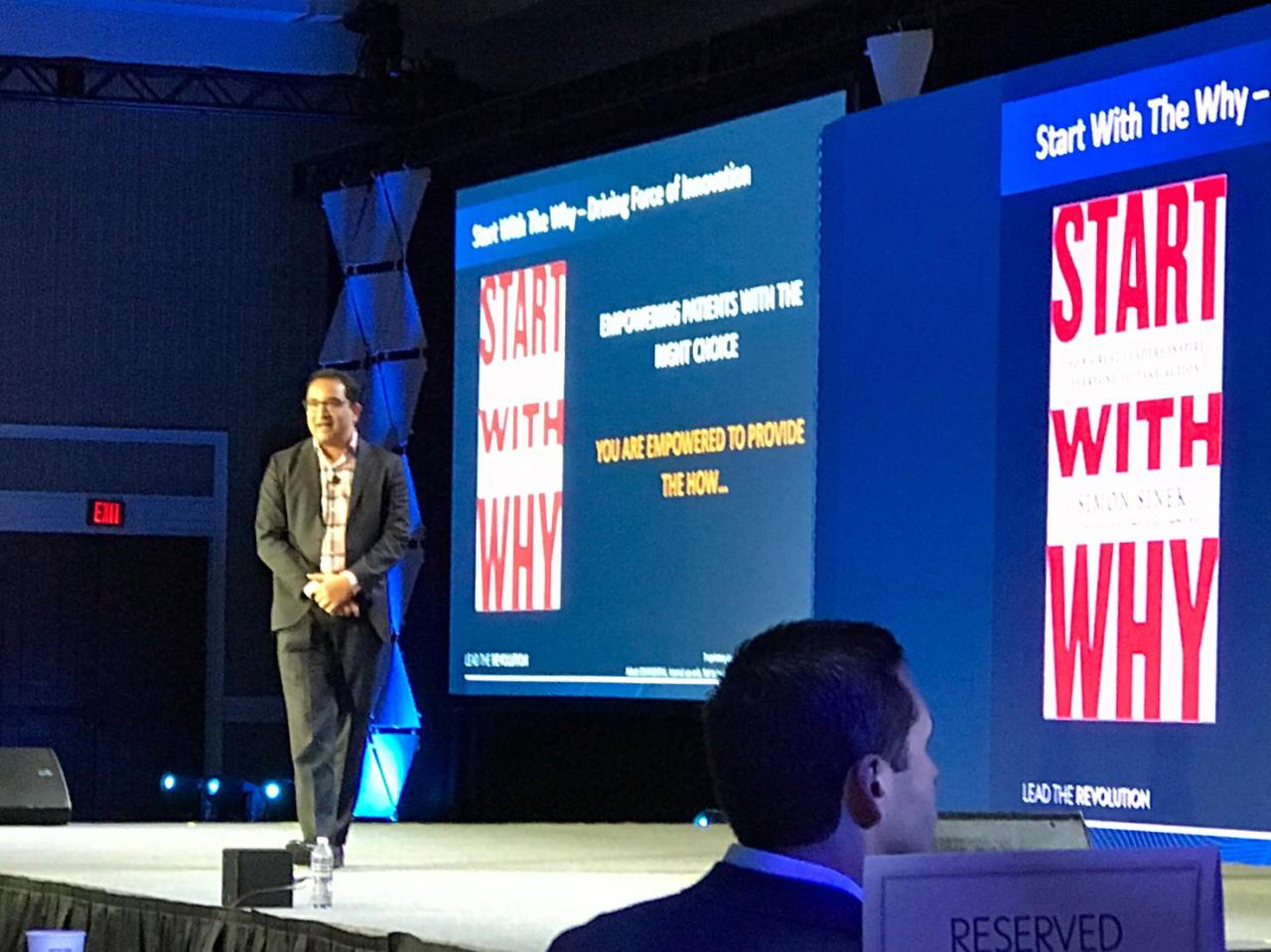
Course Director: Krishnan Chakravarthy, M.D., Ph.D.
Coastal Research Institute is launching its first patient facing, chronic pain conference “EMPOWER YOU” specializing in pain therapy options & education.
EMPOWER YOU features the following:
A high focus on patients and their ability to understand their options.
A landmark moment for its growing specialty using evidence based approaches to educate primary care providers, caregivers, and patients.
An agenda packed with educational sessions and product theaters.
Research
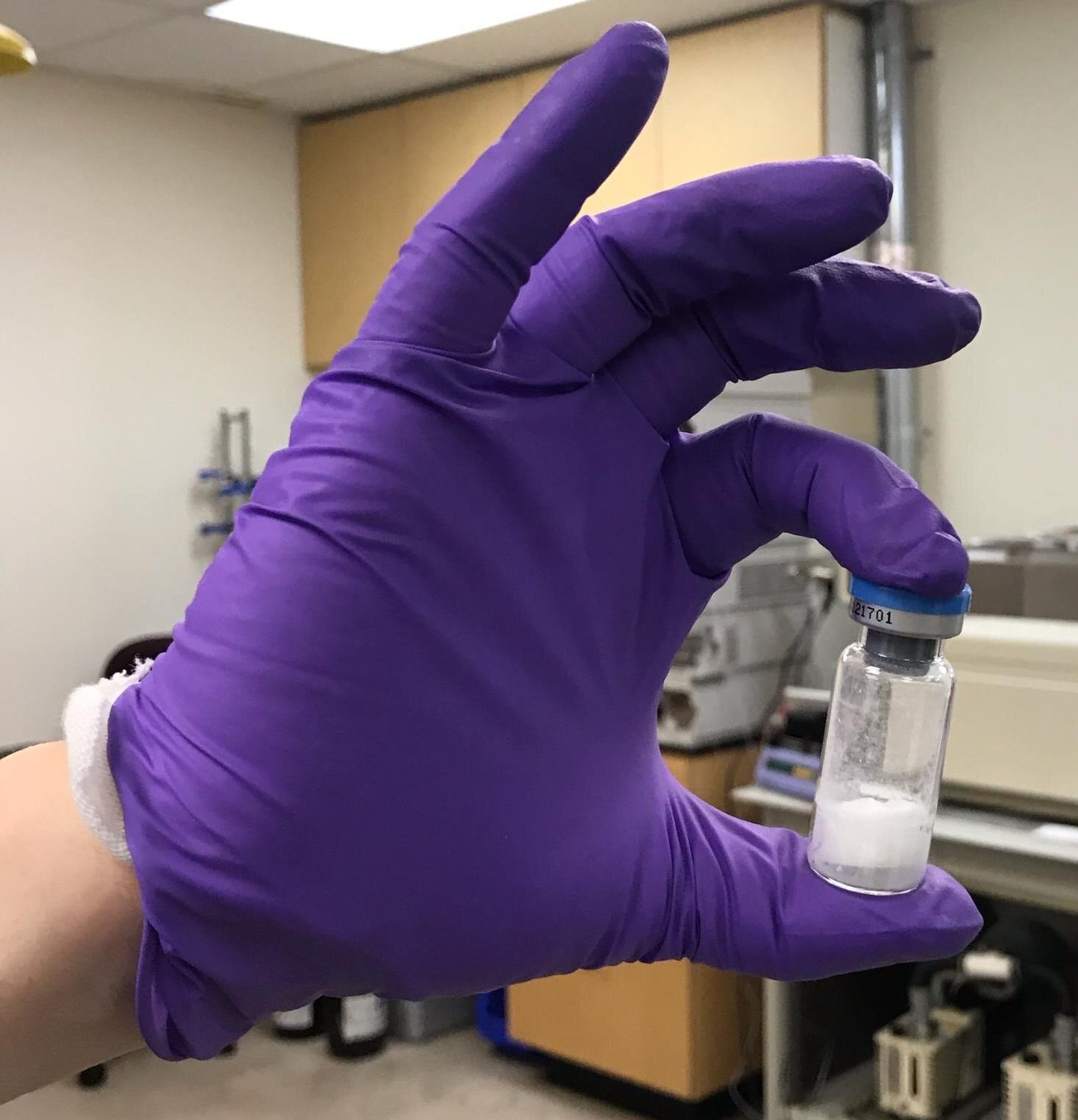
Chronic Pain and Small Molecule Drug Development
The Chakravarthy laboratory is currently working with the pharmaceutical company Eisai Pharmaceuticals, as well as the National Institute of Health, to develop novel small molecule therapies to treat chronic pain. This includes targeting Toll-Like Receptor 4 and Kindolor, which acts as an inhibitor of the pain propagating Nav1.7 and Nav1.8 sodium channels and as an inhibitor of NMDA receptors that act to magnify pain signals.
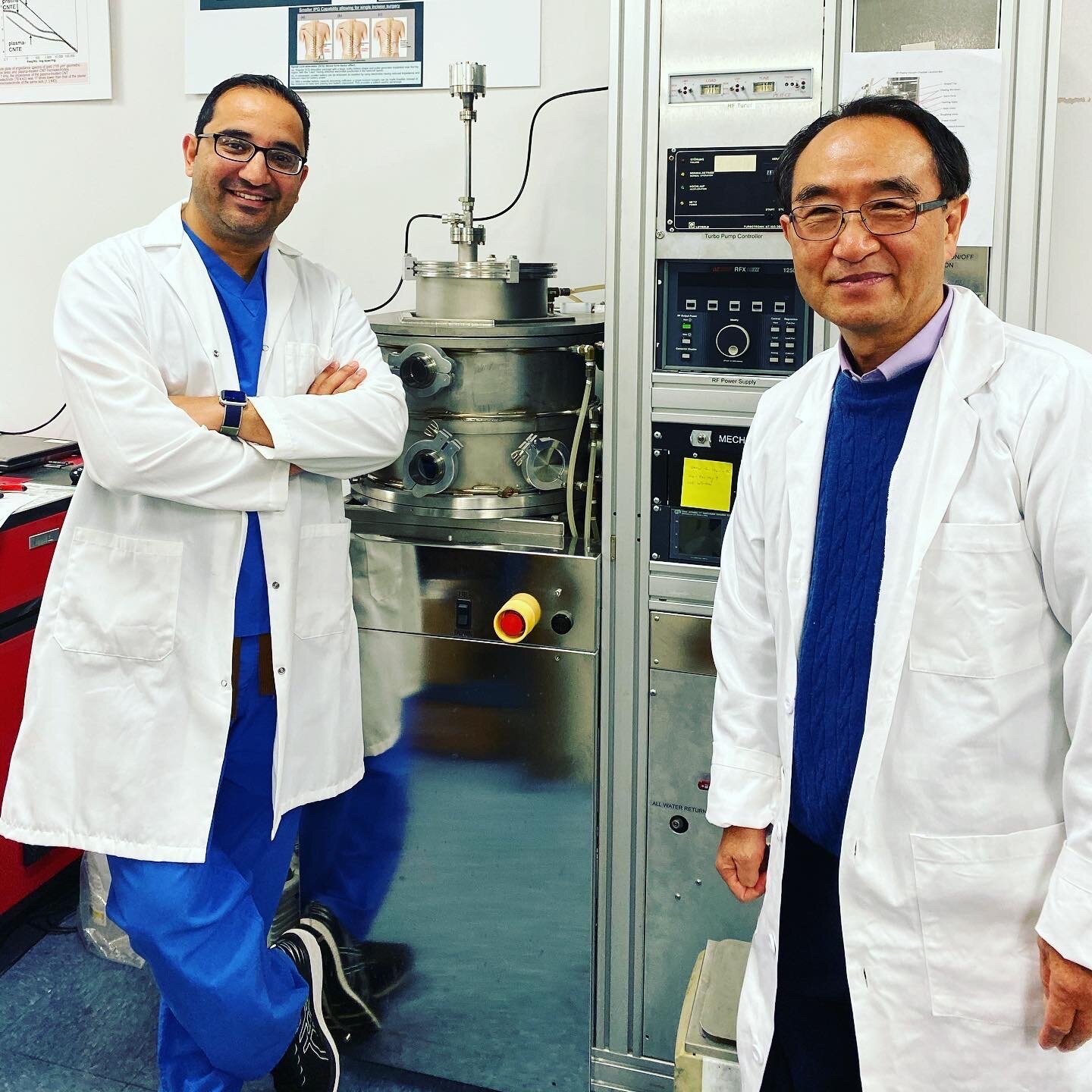
Nanomedicine
The Chakravarthy laboratory is working with the UCSD Department of NanoEngineering to advance a new microneedle-based transdermal drug delivery of pain medications and efficient vaccine delivery. This approach overcomes the deficiencies of using hypodermic needles, which have served as the primary strategy for vaccine and medication delivery, but inflict pain, incite extreme fear in varying degrees (reducing compliance), and are the causative factor in injury and infection. In addition, there is a pressing need for rapid deployment for vaccine and drug delivery and less use of medical and staff resources to achieve that delivery.
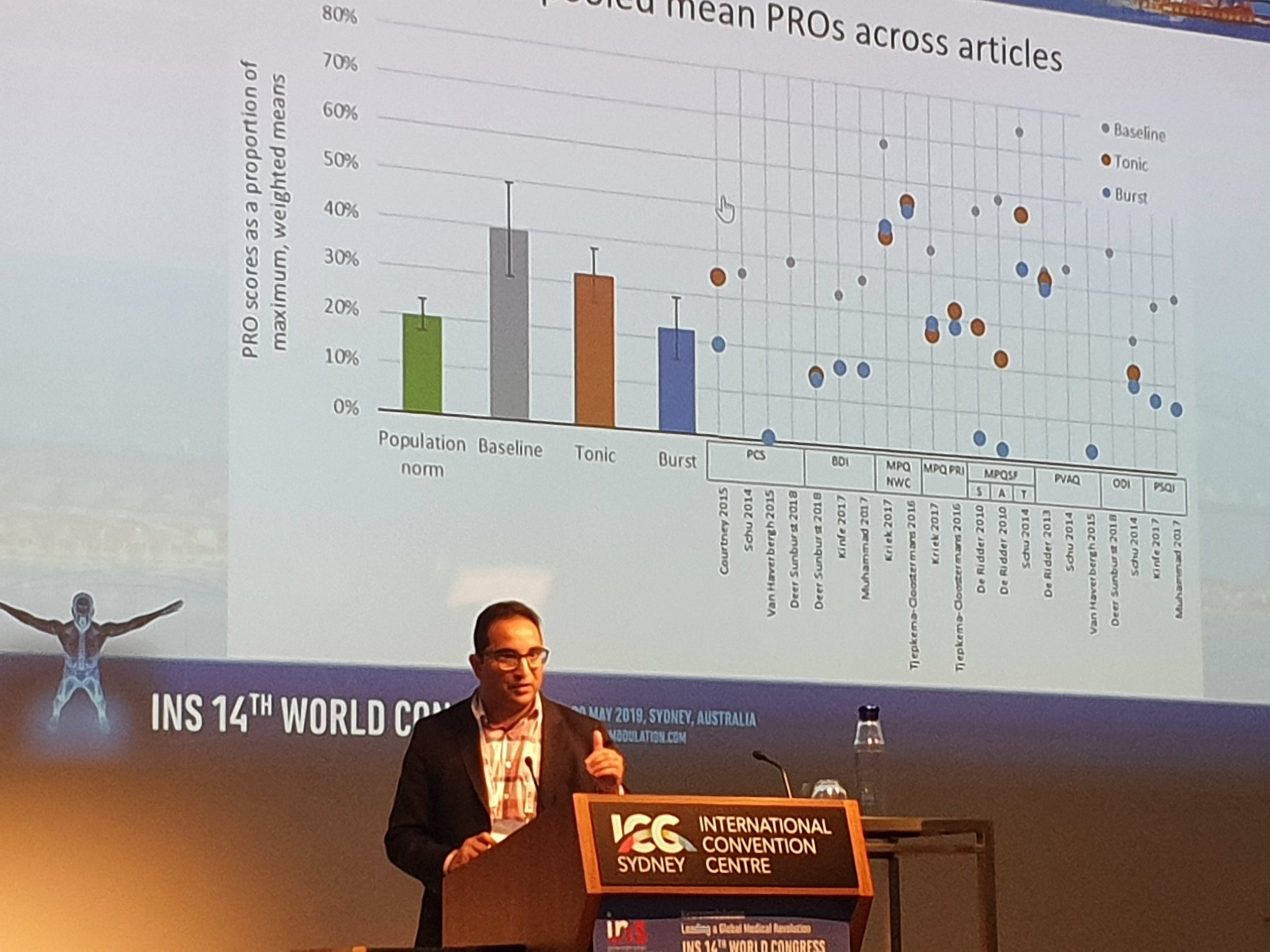
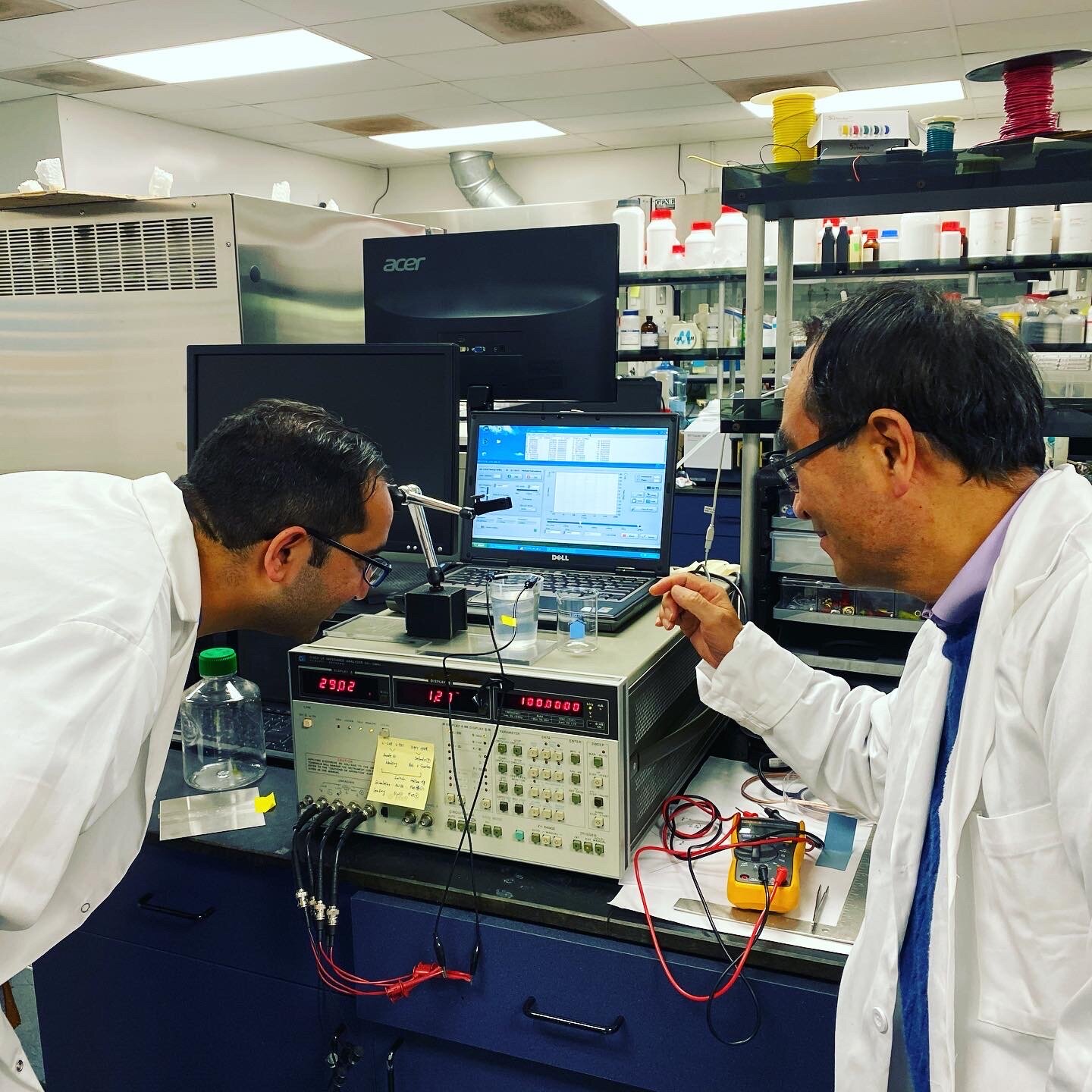
Neuromodulation
Physicians in the United States have been using spinal cord stimulation (SCS) to treat chronic pain conditions since it was first developed nearly half a century ago. Inspired by the seminal gate-control theory of pain proposed by Melzack and Wall, the conventional paradigm of SCS utilizes tonic 40-60 Hz stimulation that activates dorsal columns to elicit paresthesia over a patient’s painful region. This paresthesia-based SCS has proven to be an effective treatment modality for 40-50% of patients with refractory pain conditions, including complex regional pain syndrome and failed back surgery syndrome (FBSS). However, conventional SCS has several limitations, such as limited clinical indications, suboptimal or inadequate pain inhibition (e.g., non-responders), and progressive reduction of treatment effects over time. The Chakravarthy Laboratory in collaboration with UCSD Nanoengineering laboratory is developing new paradigm-shifting neuromodulation technology and spinal cord stimulation devices. We are also actively involved in several ongoing clinical trials with industry partners.
Clinical Trials
If you are interested in joining any of the following clinical trials, kindly contact our clinical research manager, Suzanne Nanson: ![]()

Bioventus Peripheral Nerve Registry
A Prospective, open-label, long-term, multi-center, registry to assess the safety and efficacy of the Bioness StimRouter Neuromodulation system in subjects with chronic pain of peripheral nerve origin.

Study Sponsored Registry with Vivex Biologics
Single center registry study focusing on using ViaDisc as an non-surgical treatment option for supplementing degenerated intervertebral discs. VIA Disc is an allogeneic disc tissue matrix injected into the center of the nucleus pulposus of a painful disc in a convenient and safe outpatient setting.

Study Sponsored by Rune Labs
A validation of evoked compound action potentials as an ancillary biomarker for multiple sclerosis induced demyelination and pain. A feasibility study that is an open-label study to assess the presence of data in the ECAP signal that is measured by a spinal cord stimulation (SCS) device which may correlate with demyelination in Multiple Sclerosis patients.

Study Sponsored by Mainstay Medical
The RESTORE study will compare Optimal Medical Management (OMM) to the Reactiv8 System in a prospective randomized study. This treatment will target intractable mechanical chronic low back pain. Optimal Medical Management is managed according to current guideline treatments, including medication, physical therapy, and injection. Reactiv 8 therapy is an implantable electrical stimulation system that is initiated manually by an external device.

Studies Sponsored by Abbott
DISTINCT: the Dorsal spInal cord STImulation vs mediCal management for the Treatment of low back pain (DISTINCT study) is a prospective, multicenter, randomized, controlled, post market trial. It is designed to evaluate the efficacy of BurstDR SCS compared to conventional medical management in the treatment of chronic low back pain including neuropathic pain. We are currently following up with our patients on this study and not enrolling any new patients.
T2P: Spinal Cord Stimulation trial to Permanent Prediction (SCS T2P) is a prospective, longitudinal, multi-center, non-randomized, dual arm, open-label, clinical feasibility study. This study investigates whether objective data (wearable sensors) collected from chronic pain patients coincides with the subjective patient-reported outcomes (PROs) and adjustments with SCS device.

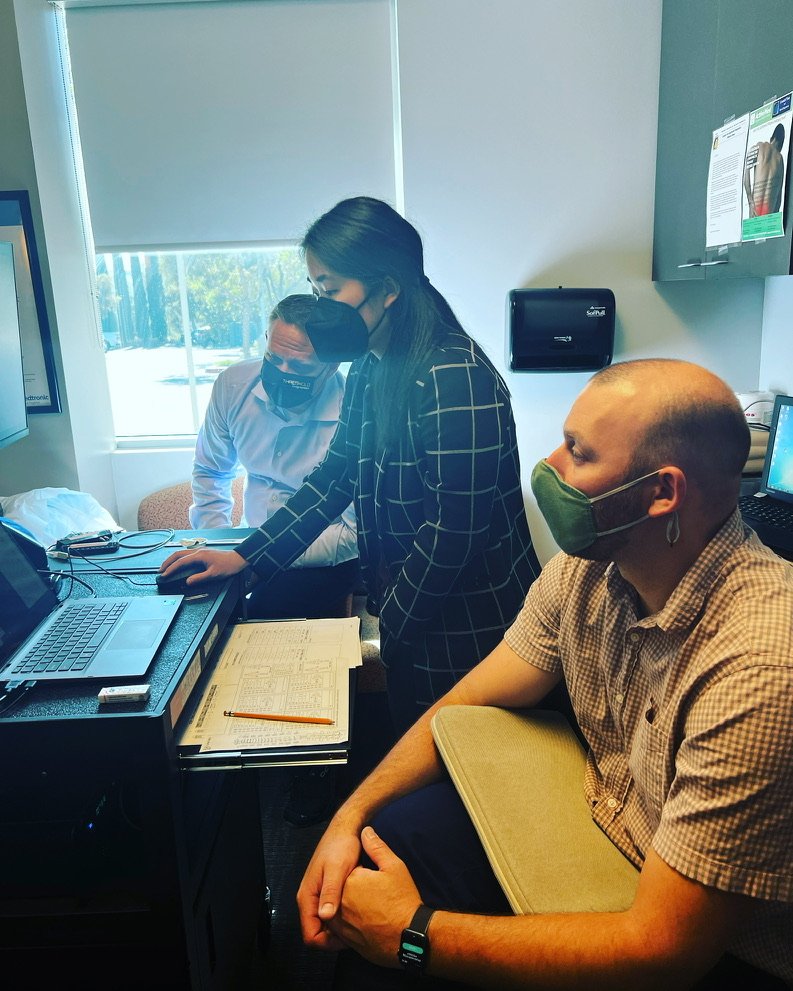
Studies Sponsored by Medtronic
PSTM: the registry is designed to conduct non-randomized, active prospective post-market surveillance. The registry design is patient-centric and follows a single patient receiving therapy from the spinal cord stimulator.
TDD: the registry is designed to conduct non-randomized, active prospective post-market surveillance. The registry design is patient-centric and follows a single patient receiving therapy from the targeted drug delivery.
Echo-MDT: electrically evoked compound action potentials human observation Medtronic system study (ECHO-MDT). This is a prospective, multi-center, nonsignificant risk IDE study of non-evoked and evoked waveforms resulting from stimulation of the dorsal column using a closed-loop system comprised of Medtronic hardware or OTS hardware, which uses recorded waveforms to adjust stimulation amplitude.

Studies Sponsored by Boston Scientific
Envision: a prospective, post-market, multi-center study whose objective is to characterize the relationship between select objective metrics and clinical outcomes in chronic pain patients treated with Boston Scientific commercially approved neurostimulation systems and may use observed relationships to make recommendations.
Scope: a prospective, multicenter, single-arm observational post-approval study to compile real-world outcomes of the Superion IDS in routine clinical practice. The Superion IDS is intended to treat skeletally mature patients suffering from pain, numbness, and/or cramping in the legs (neurogenic intermittent claudication) secondary to a diagnosis of moderate degenerative lumbar spinal stenosis.
Faculty/Sites
Solutions
CRI Research Standard of Excellence
Industry, and NIH funded clinical trial institute
Focused on small molecule, medical device development
Distinguished clinical partnership with Coastal Pain and Spinal Diagnostics
In-house toxicology laboratory for potential biomarker analysis
10,000 square foot Ambulatory Surgery Center for Clinical Work
New IP creation for potential licensing opportunities
Digital Services with a focus on objective outcomes measures
Center of Excellence Development for physician training
Industry driven pre-clinical and clinical trials research
Quality, relevant and compliant study participant selection
Good Clinical Practices
Leadership
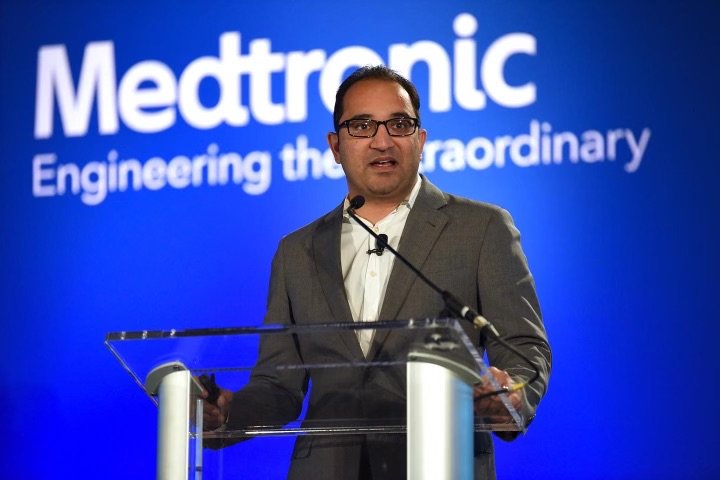
President, Executive Director of Institute
 Dr. Krishnan Chakravarthy M.D., Ph.D. has >100 papers published; >50 abstracts; >300 regional, national, and international talks; National/International Award Winner in Pain Medicine; International Thought Leader in Pain Space. He serves on the board of the major pain companies and sits on the editorial board of several national and international journals. He completed his residency at the Johns Hopkins Hospital, and pain fellowship at Harvard/Massachusetts General Hospital. He also sits on the executive board and committees of the major pain societies such as American Society of Pain and Neuroscience. Expertscape's PubMed-based algorithms placed Dr. Chakravarthy in top 0.1% of scholars writing about Pain Management over the past 10 years defining him as a "World Expert.” He has been involved in pioneering several first clinical cases in the United States and has been a founding faculty member of “Restorative Neurostimulation”. To date he has raised >9 million in direct and and indirect funding and launched multiple startups from his research work that are taking paradigm shifting technologies to market.
Dr. Krishnan Chakravarthy M.D., Ph.D. has >100 papers published; >50 abstracts; >300 regional, national, and international talks; National/International Award Winner in Pain Medicine; International Thought Leader in Pain Space. He serves on the board of the major pain companies and sits on the editorial board of several national and international journals. He completed his residency at the Johns Hopkins Hospital, and pain fellowship at Harvard/Massachusetts General Hospital. He also sits on the executive board and committees of the major pain societies such as American Society of Pain and Neuroscience. Expertscape's PubMed-based algorithms placed Dr. Chakravarthy in top 0.1% of scholars writing about Pain Management over the past 10 years defining him as a "World Expert.” He has been involved in pioneering several first clinical cases in the United States and has been a founding faculty member of “Restorative Neurostimulation”. To date he has raised >9 million in direct and and indirect funding and launched multiple startups from his research work that are taking paradigm shifting technologies to market.
Director of Institute Operations/Business Development
 Dr. Nathan A. Miller, M.D. is a pioneer in the field of pain medicine with over a decade of experience treating patients in the North County San Diego area. Dr. Nathan Miller is a well-respected, compassionate physician who strives to help his patients regain their lives. He is Chief of Pain Medicine at Scripps Memorial Hospital, Encinitas and is double-board certified in Anesthesiology and Interventional Pain Medicine. Dr. Miller completed his pain fellowship at the prestigious University Of Virginia pain program. He is a diplomat of the National Board of Medical Examiners and a Qualified Medical Examiner in the State of California. Dr. Miller is at the forefront in the treatment and management of a wide variety of acute and chronic pain disorders. He is a strong proponent of a multi-disciplinary approach in pain management to improve outcome and increase quality of life. With his knowledge and the use of advanced medicine, he has been able to help many patients who had little hope of a functional life.
Dr. Nathan A. Miller, M.D. is a pioneer in the field of pain medicine with over a decade of experience treating patients in the North County San Diego area. Dr. Nathan Miller is a well-respected, compassionate physician who strives to help his patients regain their lives. He is Chief of Pain Medicine at Scripps Memorial Hospital, Encinitas and is double-board certified in Anesthesiology and Interventional Pain Medicine. Dr. Miller completed his pain fellowship at the prestigious University Of Virginia pain program. He is a diplomat of the National Board of Medical Examiners and a Qualified Medical Examiner in the State of California. Dr. Miller is at the forefront in the treatment and management of a wide variety of acute and chronic pain disorders. He is a strong proponent of a multi-disciplinary approach in pain management to improve outcome and increase quality of life. With his knowledge and the use of advanced medicine, he has been able to help many patients who had little hope of a functional life.
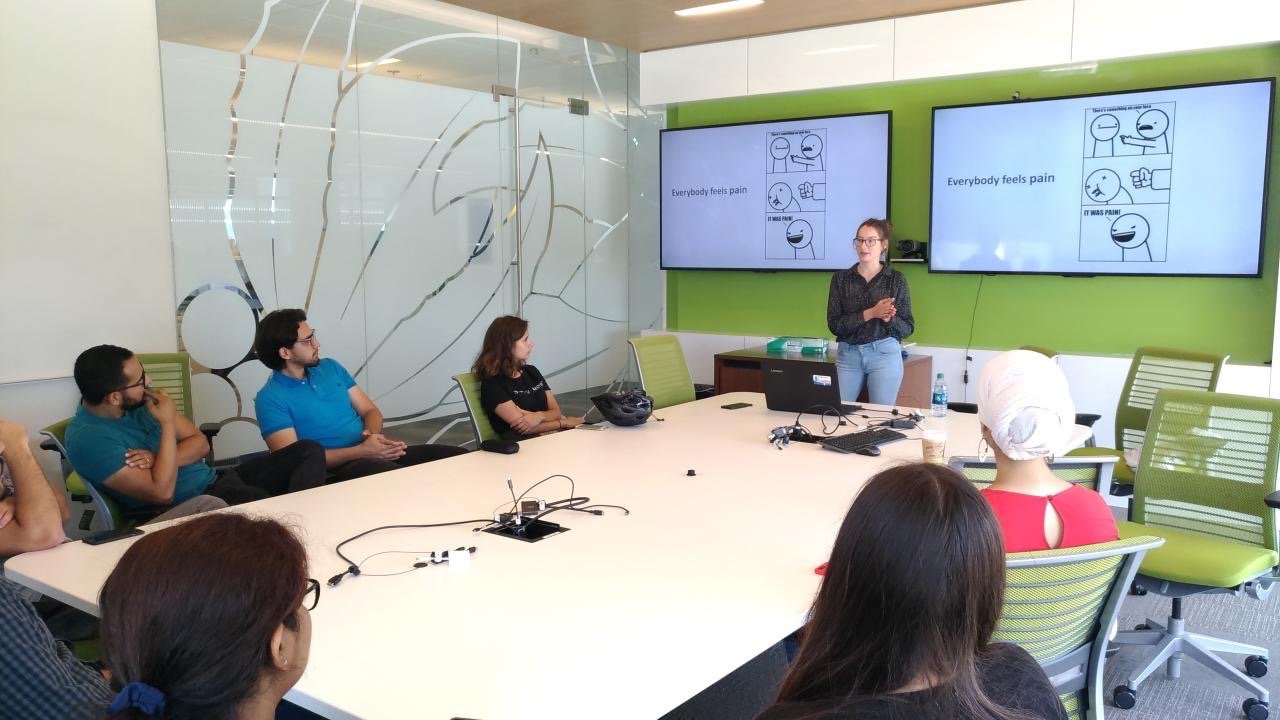
Consultant
 Dr. Moleen Madziva, Ph.D., is an award-winning leader with over 12 years experience in medical devices Clinical Research. She’s a trained Electrical, Computer and Software Engineer with extensive R&D experience whose notable contributions led to the IDE approval of the Angelmed Guardian heart monitoring device in 2018. Her clinical science work in chronic pain and neurological disorders at Abbott led to publications of post market clinical evidence for several implantable devices. Her growing expertise in Artificial Intelligence positions her as a highly sort out Clinical Affairs Advisor since cost of running clinical trials hinges on speed of quality enrollment. She is dedicated to Clinical Research because of its capacity for bridging innovation with access to lifesaving treatments for patients. Beyond her leadership roles in Clinical Affairs, Dr. Madziva also serves as mentor and advisor to students and young professionals in STEM because she’s keenly aware of the need, particularly among women of color who do not see themselves widely represented in this industry. She’s well respected among her peers and brings inspiration and joy to everyone she meets.
Dr. Moleen Madziva, Ph.D., is an award-winning leader with over 12 years experience in medical devices Clinical Research. She’s a trained Electrical, Computer and Software Engineer with extensive R&D experience whose notable contributions led to the IDE approval of the Angelmed Guardian heart monitoring device in 2018. Her clinical science work in chronic pain and neurological disorders at Abbott led to publications of post market clinical evidence for several implantable devices. Her growing expertise in Artificial Intelligence positions her as a highly sort out Clinical Affairs Advisor since cost of running clinical trials hinges on speed of quality enrollment. She is dedicated to Clinical Research because of its capacity for bridging innovation with access to lifesaving treatments for patients. Beyond her leadership roles in Clinical Affairs, Dr. Madziva also serves as mentor and advisor to students and young professionals in STEM because she’s keenly aware of the need, particularly among women of color who do not see themselves widely represented in this industry. She’s well respected among her peers and brings inspiration and joy to everyone she meets.
Director of International Outreach
 Dr. Dan Bates, M.D. is a Sports and Exercise Medicine Specialist. He is the Managing Director at Metro Pain Group and Metro Pain Research Institute and is the Chairman of the Board at Moans House Private Hospital.
Dr. Dan Bates, M.D. is a Sports and Exercise Medicine Specialist. He is the Managing Director at Metro Pain Group and Metro Pain Research Institute and is the Chairman of the Board at Moans House Private Hospital.
Dr Bates works full time with people suffering back, neck and joint pain. Prior to this he worked extensively in Sports Medicine for multiple professional and national sporting teams. He was the head doctor at Australian Football League teams Melbourne and North Melbourne.
Dr Bates’ research career has been broad covering exercise induced asthma, examination techniques, biologics, osteoarthritis, chronic pain and neuromodulation. He is the Managing Director of Metro Pain Research Institute which runs multiple first-in-man studies in pain.
He lectures nationally and internationally regularly, has 3 kids and the worlds most tolerant wife.
Director of Clinical Operations and Outreach
 Yogesh V. Patel, M.D. (“Dr. Yogi Patel”) has dedicated his life to the eradication of pain. Dr. Yogesh Patel practices evidence based medicine and the multi-disciplinary approach to pain management, giving his patients the most options and the best care possible. He has helped many patients with difficult and advanced debilitating pain conditions. Dr. Patel is double board certified in Anesthesiology and Interventional Pain Medicine from the American Board of Anesthesiology. Dr. Patel is admired by his colleagues and adored by his patients. Dr. Patel trained at UCSD, one of the highest rated interventional pain fellowship programs in the country. Dr. Patel is the founder of MyPainTools, a chronic pain education and prevention program. He feels that knowledge is empowerment, and that educated patients have the best chance for a pain-free lifestyle. Along with MyPainTools, he is actively developing programs to bring support groups and community education opportunities to North County. Dr. Patel has also worked extensively with other physicians and has placed strong emphasis on developing a strong working relationship with referring physicians with the end result of providing excellent and timely patient care.
Yogesh V. Patel, M.D. (“Dr. Yogi Patel”) has dedicated his life to the eradication of pain. Dr. Yogesh Patel practices evidence based medicine and the multi-disciplinary approach to pain management, giving his patients the most options and the best care possible. He has helped many patients with difficult and advanced debilitating pain conditions. Dr. Patel is double board certified in Anesthesiology and Interventional Pain Medicine from the American Board of Anesthesiology. Dr. Patel is admired by his colleagues and adored by his patients. Dr. Patel trained at UCSD, one of the highest rated interventional pain fellowship programs in the country. Dr. Patel is the founder of MyPainTools, a chronic pain education and prevention program. He feels that knowledge is empowerment, and that educated patients have the best chance for a pain-free lifestyle. Along with MyPainTools, he is actively developing programs to bring support groups and community education opportunities to North County. Dr. Patel has also worked extensively with other physicians and has placed strong emphasis on developing a strong working relationship with referring physicians with the end result of providing excellent and timely patient care.
Treasurer
 Dr. Ankush Bansal, M.D., is a double board-certified Anesthesiologist and Interventional Pain Physician (through the American Board of Anesthesiology) that has devoted his career to understanding complex and difficult-to-treat painful conditions. He has helped numerous patients with incapacitating pain improve their quality of life and regain function. He is actively involved in ongoing clinical research and multiple national medical societies including American Society of Interventional Pain Physicians, American Society of Regional Anesthesia, and North American Neuromodulation Society. He has published articles in peer-reviewed medical journals including the Pain Medicine Journal. He is continually striving to find new and effective ways to treat chronic pain. He completed his Doctor of Medicine (MD) at the University of Michigan Medical School. After enduring a chronic painful neck injury, he moved to Los Angeles to specialize in Anesthesiology and Chronic Interventional Pain Management through the University of California Los Angeles (UCLA) where he was mentored by some of the most renown figures in the field of Pain Medicine.
Dr. Ankush Bansal, M.D., is a double board-certified Anesthesiologist and Interventional Pain Physician (through the American Board of Anesthesiology) that has devoted his career to understanding complex and difficult-to-treat painful conditions. He has helped numerous patients with incapacitating pain improve their quality of life and regain function. He is actively involved in ongoing clinical research and multiple national medical societies including American Society of Interventional Pain Physicians, American Society of Regional Anesthesia, and North American Neuromodulation Society. He has published articles in peer-reviewed medical journals including the Pain Medicine Journal. He is continually striving to find new and effective ways to treat chronic pain. He completed his Doctor of Medicine (MD) at the University of Michigan Medical School. After enduring a chronic painful neck injury, he moved to Los Angeles to specialize in Anesthesiology and Chronic Interventional Pain Management through the University of California Los Angeles (UCLA) where he was mentored by some of the most renown figures in the field of Pain Medicine.
Staff
Advisory Board
 Dr. Timothy Deer, M.D. received his medical degree from the West Virginia University School of Medicine, and received his training in Anesthesiology and Pain Medicine at The University of Virginia. Dr. Deer is the President and Chief Executive Officer of The Spine and Nerve Center of the Virginias in Charleston, West Virginia. The Center focuses on pivotal research and the algorithmic application of Neuromodulation therapies to improve pain and function. Dr. Deer is the founder and Chairman of the American Society of Pain and Neuroscience and Immediate Past President of the International Neuromodulation Society (INS) and is President Emeritus of the West Virginia Society of Interventional Pain Physicians. Dr Deer is a past Chairman of the Pain Committee of the American Society of Anesthesiologists (ASA). He has published over 200 peer reviewed manuscripts, several book chapters and several widely used text books. Dr. Deer has taught interventional techniques throughout North America, South America, Australia, Asia, and Europe. He continues to focus on landmark research to advance the field of Neuromodulation. His latest book, Deer's Treatment of Pain is currently being used as an anchor of pain treatment information throughout the world.
Dr. Timothy Deer, M.D. received his medical degree from the West Virginia University School of Medicine, and received his training in Anesthesiology and Pain Medicine at The University of Virginia. Dr. Deer is the President and Chief Executive Officer of The Spine and Nerve Center of the Virginias in Charleston, West Virginia. The Center focuses on pivotal research and the algorithmic application of Neuromodulation therapies to improve pain and function. Dr. Deer is the founder and Chairman of the American Society of Pain and Neuroscience and Immediate Past President of the International Neuromodulation Society (INS) and is President Emeritus of the West Virginia Society of Interventional Pain Physicians. Dr Deer is a past Chairman of the Pain Committee of the American Society of Anesthesiologists (ASA). He has published over 200 peer reviewed manuscripts, several book chapters and several widely used text books. Dr. Deer has taught interventional techniques throughout North America, South America, Australia, Asia, and Europe. He continues to focus on landmark research to advance the field of Neuromodulation. His latest book, Deer's Treatment of Pain is currently being used as an anchor of pain treatment information throughout the world.
 Dr. Joseph Wang, Ph.D. is an American researcher and inventor. He is a Distinguished Professor, SAIC Endowed Chair, and former Chair of the Department of Nanoengineering at the University of California, San Diego specializing in nanomachines, biosensors, nano-bioelectronics, wearable devices, and electrochemistry. He also serves as the Director of the Center for Wearable Sensors at the University of California San Diego Jacobs School of Engineering.
Dr. Joseph Wang, Ph.D. is an American researcher and inventor. He is a Distinguished Professor, SAIC Endowed Chair, and former Chair of the Department of Nanoengineering at the University of California, San Diego specializing in nanomachines, biosensors, nano-bioelectronics, wearable devices, and electrochemistry. He also serves as the Director of the Center for Wearable Sensors at the University of California San Diego Jacobs School of Engineering.
 Dr. Ricardo Vallejo, M.D., Ph.D. is the Director of Research at Millennium Pain Center. He is deeply committed to discovering new methods and treatments for chronic pain. Dr. Vallejo holds multiple appointments in the editorial boards of international peer review journals such as Clinical Journal of Pain, Pain Physicians, Journal of Opioid Management Revista Mexicana de Anestesiologia. Dr. Vallejo is the current Associate Editor of the journal Pain Practice, where he established the section Images in Pain Practice in 2007. He is also a member of the examination board for the World Institute of Pain. Dr. Vallejo has published extensively in national and international peer-review journals and serves as a speaker in meetings around the world. He is adjunct professor at the Illinois State University. Research interests of Dr. Vallejo include management of chronic pain status, such as sympathetically maintained pain: failed back surgery, and discogenic low back pain. His research efforts are aimed at understanding the immune mechanisms underlying neuropathic pain conditions and the effects of electrical stimulation on the central and peripheral immune response.
Dr. Ricardo Vallejo, M.D., Ph.D. is the Director of Research at Millennium Pain Center. He is deeply committed to discovering new methods and treatments for chronic pain. Dr. Vallejo holds multiple appointments in the editorial boards of international peer review journals such as Clinical Journal of Pain, Pain Physicians, Journal of Opioid Management Revista Mexicana de Anestesiologia. Dr. Vallejo is the current Associate Editor of the journal Pain Practice, where he established the section Images in Pain Practice in 2007. He is also a member of the examination board for the World Institute of Pain. Dr. Vallejo has published extensively in national and international peer-review journals and serves as a speaker in meetings around the world. He is adjunct professor at the Illinois State University. Research interests of Dr. Vallejo include management of chronic pain status, such as sympathetically maintained pain: failed back surgery, and discogenic low back pain. His research efforts are aimed at understanding the immune mechanisms underlying neuropathic pain conditions and the effects of electrical stimulation on the central and peripheral immune response.
Startups

Douleur Therapeutics is a clinical-stage pharmaceutical company located in San Diego, CA, that is focused on revolutionizing the treatment of neuropathic pain. Our compound, DT-001, is a TLR-4 antagonist and has been shown to be safe in over 1500 patients. Our strategy is to apply DT-001 to Chronic Post-Operative Pain (CPOP). Extensive pre-clinical data indicate that overstimulation of TLR-4 can place the immune system into overdrive causing acute pain to transition into chronic pain. Other potential therapeutic areas are: joint pain, discogenic pain, chemotherapy-induced peripheral neuropathy, migraines, and the propagation of opioid-induced hyperalgesia pathway.

Newrom Biomedical aims to revolutionize the Neurostimulation paradigm using nanotechnology to achieve optimized patient-centric outcomes. We are a startup company located in San Diego, CA, specialized in next-generation spinal cord stimulation and dorsal root ganglion stimulation development.

Next Generation Stimulation Technologies (NXTSTIM) was founded by Dr. Krishnan Chakravarthy MD, PhD in 2020. NXTSTIM is an American neuromodulation & biotechnology company based in San Diego, California, United States. NXTSTIM designs & manufactures medical devices leveraging disruptive battery technology, AI & ML software platforms.

Creating a solution to a major problem in todays $2.6 billion global SCS marketplace. The issue of SCS trial lead migration effects every physicians practice knowingly or unknowingly. As an industry there is no consistency or continuity on how to anchor SCS Trial leads. Accufix Medical was founded to commercialize Stimfix as an Novel Anchoring Technology developed to address this issue.
Paravertebral Closed Loop Muscle Stimulator
First distributed in the 1960s, spinal cord stimulation (SCS) utilized artificially generated electricity to modulate human tissue that relied on electricity to propagate signals. Since then, a closed-loop system was developed which utilizes recorded evoked compound action potentials (ECAPs) to a fixed-output, open-loop system for patients with chronic back and leg pain. A self-adjusting SCS system can internally preserve optimal programming parameters while adapting to the patient’s experiences or activities. Closed-looped stimulation provides neuromodulators, for the first time ever, with the ability to objectively measure and interact with the spinal cord’s electrical activity, just like a cardiac pacemaker would with the heart. The implications of this concept are the most progress science has made in the potential for providing superior pain control with SCS.
News
2022
2021
Spinal Cord Stimulation Reduces Pain and Motor Symptoms in Parkinson’s Disease Patients
Qualcomm Institute-based Startup Receives Funding to Continue Development of Opioid Sensor
Tackling Both Physical and Psychological Pain
2010-2019
UC San Diego Health Offers New Bluetooth-Enabled “Pacemaker” for Chronic Focal Nerve Pain
Intrathecal Drug Delivery and Spinal Cord Stimulation for Cancer Pain: A Review
Spinal cord stimulation and chronic pain: In the end it’s about the patient
Study in Mice Suggests How Anesthesia May Fight Lung Infections
Scientists find new benefit from inhaled anesthetics to effectively combat lung infections
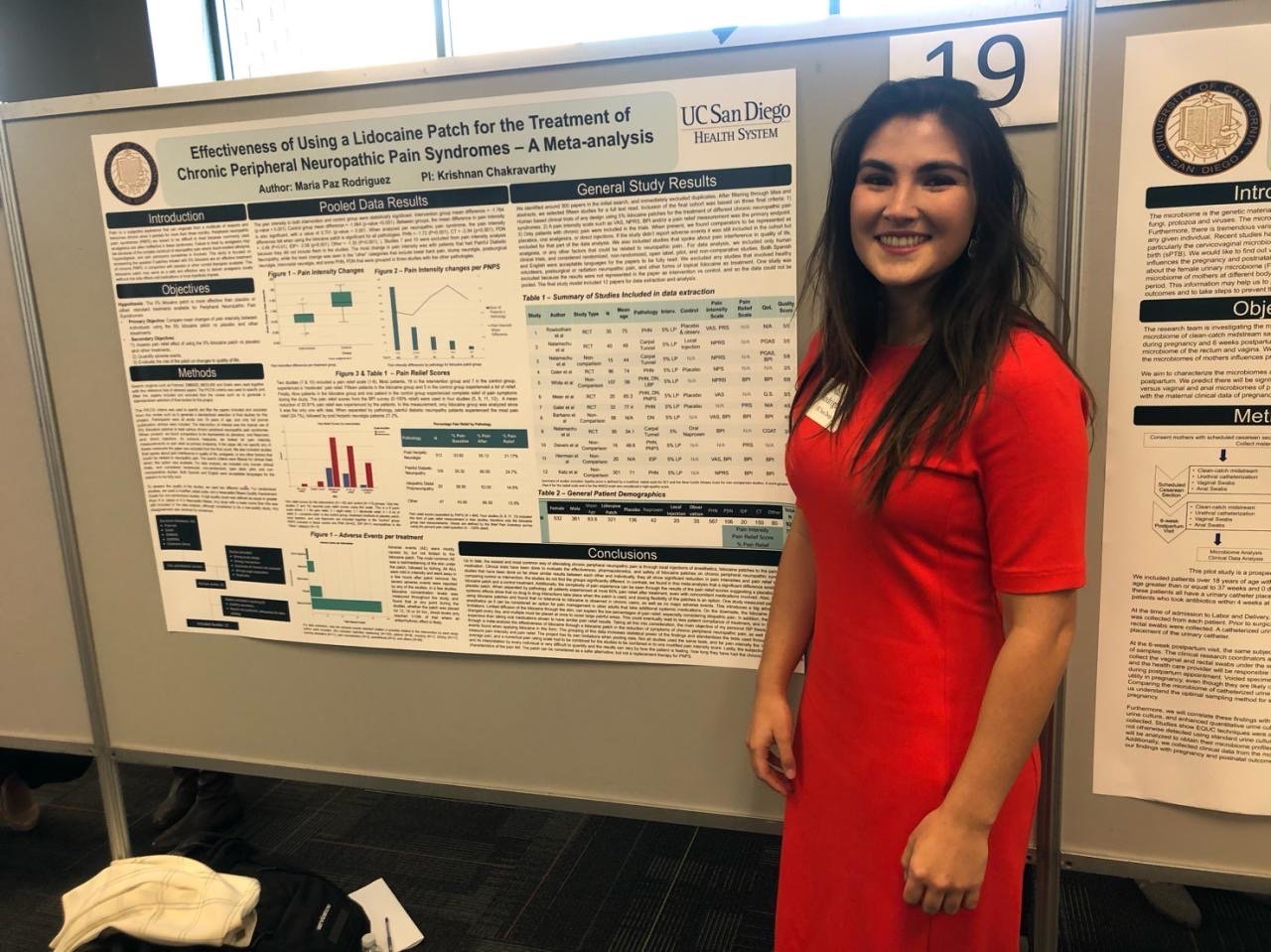
Alumni
Farzan Vahedifard
Lakshmi Rekha Narra
Dr. Rajiv Reddy
Wathnita Sarik
Rahul Chaturvedi
Coastal Research Institute
6221 Metropolitan Street, Ste. 201
Carlsbad, CA 92009
phone: (760) 607-1729
Contact Us
We look forward to hearing from you. Please allow up to 1-2 business days for a response from one of our representatives.